In an evolving health landscape, emerging research continues to highlight concerns that could impact everyday wellbeing. Here’s the key update you should know about:
Scientists from Trinity College Dublin have discovered that electrically stimulating “macrophages” – one of the immune systems key players – can “reprogram” them in such a way to reduce inflammation and encourage faster, more effective healing in disease and injury.
This breakthrough uncovers a potentially powerful new therapeutic option, with further work ongoing to delineate the specifics.
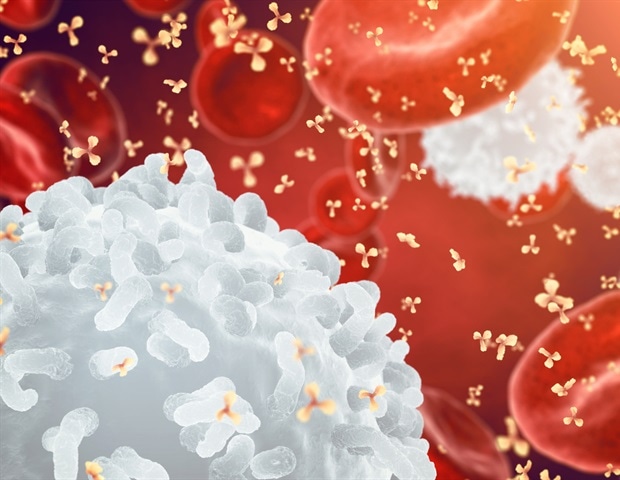
Macrophages are a type of white blood cell with several high-profile roles in our immune system. They patrol around the body, surveying for bugs and viruses, as well as disposing of dead and damaged cells, and stimulating other immune cells – kicking them into gear when and where they are needed.
However, their actions can also drive local inflammation in the body, which can sometimes get out of control and become problematic, causing more damage to the body than repair. This is present in lots of different diseases, highlighting the need to regulate macrophages for improved patient outcomes.
In the new study, just published in the international journal Cell Reports Physical Science, the Trinity team worked with human macrophages isolated from heathy donor blood samples provided via the Irish Blood Transfusion Board, St James’s Hospital. They stimulated these cells using a custom bioreactor to apply electrical currents and measured what happened.
The scientists discovered that this stimulation caused a shift of macrophages into an anti-inflammatory state that supports faster tissue repair; a decrease in inflammatory marker (signalling) activity; an increase in expression of genes that promote the formation of new blood vessels (associated with tissue repair as new tissues form); and an increase in stem cell recruitment into wounds (also associated with tissue repair).
We have known for a very long time that the immune system is vital for repairing damage in our body and that macrophages play a central role in fighting infection and guiding tissue repair.”
Dr. Sinead O’Rourke, Research Fellow in Trinity’s School of Biochemistry and Immunology, and first author of the research article
“As a result, many scientists are exploring ways to ‘reprogram’ macrophages to encourage faster, more effective healing in disease and to limit the unwanted side-effects that come with overly aggressive inflammation. And while there is growing evidence that electrical stimulation may help control how different cells behave during wound healing, very little was known about how it affects human macrophages prior to this work.”
“We are really excited by the findings. Not only does this study show for the first time that electrical stimulation can shift human macrophages to suppress inflammation, we have also demonstrated increased ability of macrophages to repair tissue, supporting electrical stimulation as an exciting new therapy to boost the body’s own repair processes in a huge range of different injury and disease situations.”
The findings from the interdisciplinary team led by Trinity investigators, Professor Aisling Dunne (School of Biochemistry and Immunology) and Professor Michael Monaghan (School of Engineering) is especially significant given that this work was performed with human blood cells (showing its effectiveness for real patients), electrical stimulation is relatively safe and easy in the scheme of therapeutic options, and the outcomes should be applicable to a wide range of scenarios.
Corresponding author Prof. Monaghan added: “Among the future steps are to explore more advanced regimes of electrical stimulation to generate more precise and prolonged effects on inflammatory cells and to explore new materials and modalities of delivering electric fields. This concept has yielded compelling effects in vitro and has huge potential in a wide range of inflammatory diseases.”
Source:
Journal reference:
O’Rourke, S. A., et al. (2025). Electromodulation of human monocyte-derived macrophages drives a regenerative phenotype and impedes inflammation. Cell Reports Physical Science. doi.org/10.1016/j.xcrp.2025.102795

