In an evolving health landscape, emerging research continues to highlight concerns that could impact everyday wellbeing. Here’s the key update you should know about:
A new study reveals that SARS-CoV-2 mRNA vaccines can amplify immune checkpoint therapy in lung and skin cancers by unleashing a potent interferon-driven immune surge that transforms resistant tumors into immunotherapy-ready targets.
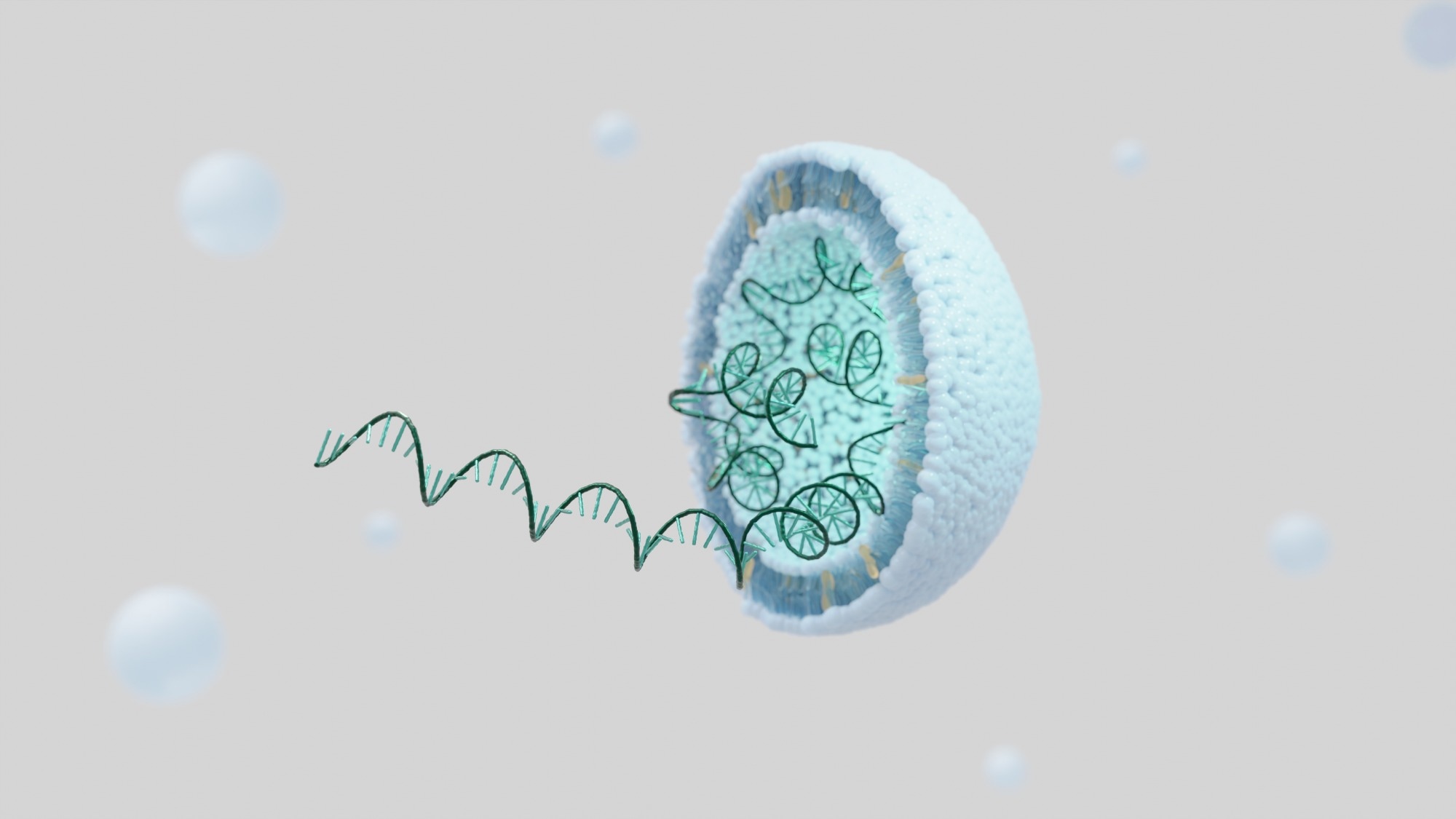
Study: SARS-CoV-2 mRNA vaccines sensitize tumours to immune checkpoint blockade. Image Credit: KwangSoo Kim / Shutterstock
In a recent study in the journal Nature, researchers investigated whether SARS-CoV-2 mRNA vaccines could sensitize cancerous tumors to immune checkpoint inhibitors (ICIs) in patients with melanoma and non-small cell lung cancer (NSCLC). The study leveraged several extensive human datasets and found that COVID-19 vaccination within 100 days of starting ICI treatment was associated with improved survival in retrospective single-institution cohorts of melanoma and NSCLC patients.
Notably, preclinical models revealed that the vaccine triggers a massive type-I interferon surge, with anti-tumor effects dependent on signaling through the type-I interferon receptor (IFNAR1), a mechanism known to prime the body’s T-cells to attack cancerous tumors. This interferon-driven response also promoted epitope spreading, in which activated T cells recognize multiple tumor antigens, and led tumors to upregulate PD-L1 as a counterdefense, rendering them newly susceptible to ICI therapy. These findings suggest that widely available, “off-the-shelf” mRNA vaccines could offer a practical, hypothesis-generating strategy to enhance ICI responses, pending further clinical validation.
Background
Immune checkpoint inhibitors (ICIs) are revolutionary anti-cancer interventions that harness the body’s immune system to fight tumors. These elements block checkpoint proteins, off switches that prevent the immune system from attacking healthy cells. By blocking these checkpoints, ICIs enable immune cells (e.g., T cells) to recognize and eliminate cancer cells more effectively. Unfortunately, while ICIs are highly effective in improving cancer outcomes and survival rates, this only works for a fraction of patients.
For most others, research suggests that the immune system fails to recognize the tumor as a threat, a mechanism termed “immunologically cold” tumors. These tumors lack the pre-existing T-cells that ICIs need to activate, rendering the therapy ineffective.
To address these cold tumors, researchers have been developing and pilot-testing personalized mRNA cancer vaccines to heat them up by teaching T cells to find them. While these approaches show promise, their manufacturing processes are complex, expensive, and time-intensive, necessitating more readily accessible, cost-effective “off-the-shelf” alternatives.
About the study
The present study addresses this pressing need and supports future cancer therapy by leveraging a multi-pronged approach that combines human patient data, preclinical animal models, and a study in healthy volunteers to investigate whether COVID-19 vaccines could replicate personalized mRNA cancer vaccines by heating cold tumors.
The study first analyzed patient records from The University of Texas MD Anderson Cancer Center, identifying patients with advanced non-small cell lung cancer (NSCLC) and metastatic melanoma who were treated with ICIs. ICI-treated patient outcomes were evaluated to elucidate whether the outcomes of those who received an mRNA COVID-19 vaccine within 100 days of starting their ICI treatment (n = 180 NSCLC patients and 43 melanoma patients) were different from those who did not (n = 704 NSCLC patients and 167 melanoma patients) to evaluate the difference in overall survival (OS) across both treatments.
The study then used preclinical murine models of known “cold” tumors (melanomas and lung cancers) to elucidate the mechanisms underlying COVID-19 vaccines’ ability to heat cold tumors. Specifically, mice were treated with a lab-made version of the Pfizer vaccine (Spike RNA-LNPs), an ICI (anti-PD-1), or a combination of both. Blocking antibodies targeting IFNAR1 (the type I interferon receptor), but not IL-1R, were used to pinpoint the immune pathway responsible for the synergistic response.
Finally, the study conducted a human mechanistic study in which blood collected from healthy volunteers (5 receiving Moderna, 11 receiving Pfizer) at multiple time points before and after vaccination was analysed using high-sensitivity assays to measure changes in over 250 immune-related cytokines. Although exploratory due to small cohort size, the analysis revealed a dose-dependent interferon response, with Moderna’s higher mRNA dose producing a somewhat stronger IFN-α signal.
Study findings
The study found that COVID-19 vaccination substantially improved patient outcomes. In the NSCLC cohort, patients who received a vaccine within 100 days of ICI treatment had a 3-year overall survival rate of 55.7%, compared with 30.8% in the unvaccinated group. Notably, this translates to a 49% reduction in cancer-associated mortality risk (adjusted hazard ratio [HR] = 0.51, p < 0.0001).
Encouragingly, COVID-19 vaccination was associated with a greater benefit in metastatic melanoma patients, with the vaccinated group demonstrating a three-year overall survival of 67.6% versus 44.1% in the unvaccinated group (HR = 0.37, p = 0.0048). This group also saw a significant improvement in progression-free survival (HR = 0.63, p = 0.0383).
Importantly, no comparable survival benefit was observed with influenza or pneumococcal vaccines, and the association persisted after correction for immortal-time bias and propensity score matching. Notably, the benefit was extended to PD-L1-low or “cold” NSCLC tumors, which typically respond poorly to ICI therapy, suggesting that the vaccine may help overcome innate resistance.
Results from the mechanism studies revealed that COVID-19 vaccines trigger a massive, viraemia-like surge of type-I interferons. Analyses of immune-related cytokines revealed that IFN-α was the most upregulated cytokine, demonstrating a 280-fold increase in only 24 hours following vaccination. This IFN surge activates the body’s innate immune system, priming T-cells to recognize and attack tumor-associated antigens (not viruses). The resulting T-cell infiltration prompts tumors to increase PD-L1 expression, a defensive adaptation that is subsequently neutralized by ICI blockade, thereby sustaining anti-tumor immunity. Blocking the type-I interferon receptor (IFNAR1) abolished the observed anti-tumor synergy in mice, confirming the pathway’s causal role.
Conclusions
The present study demonstrated that clinically available mRNA vaccines, even those targeting non-tumor antigens (like COVID-19), are potent immune modulators that may sensitize tumors to ICIs through type-I IFN-driven innate activation and epitope spreading. These findings suggest that “off-the-shelf” vaccines could represent a practical, potentially scalable approach to turning cold tumors hot, overcoming a significant barrier to effective cancer treatment. However, the authors emphasize that these findings are observational and hypothesis-generating, requiring prospective clinical validation before therapeutic adoption.
Journal reference:
- Grippin, A. J., Marconi, C., Copling, S., Li, N., Braun, C., Woody, C., Young, E., Gupta, P., Wang, M., Wu, A., Jeong, S. D., Soni, D., Weidert, F., Xie, C., Goldenberg, E., Kim, A., Zhao, C., DeVries, A., Castillo, P., … Lin, S. H. (2025). SARS-CoV-2 mRNA vaccines sensitize tumours to immune checkpoint blockade. Nature. DOI: 10.1038/s41586-025-09655-y. https://www.nature.com/articles/s41586-025-09655-y

