In an evolving health landscape, emerging research continues to highlight concerns that could impact everyday wellbeing. Here’s the key update you should know about:
In a new study led by the University of Pennsylvania School of Veterinary Medicine (Penn Vet) and Children’s Hospital of Philadelphia (CHOP), researchers found that mitochondrial dysfunction in the blood-brain barrier (BBB) may lead to neuropsychiatric disease in some patients with 22qDS. The researchers also demonstrated that a class of FDA-approved cholesterol drugs could potentially be repurposed to treat this dysfunction. These encouraging findings were published today in the journal Science Translational Medicine.
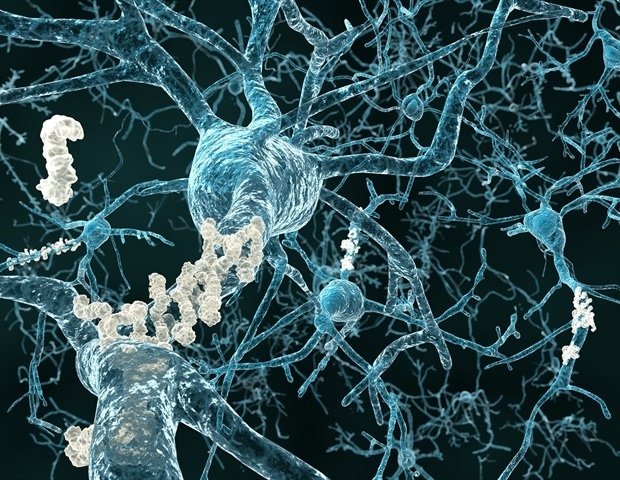
The BBB is a specialized vascular system that separates the brain from the rest of the body. Maintenance of the BBB is fundamental for optimal brain function, and BBB impairments have been linked to multiple neurological disorders, ranging from autism and schizophrenia to neurodegenerative conditions including multiple sclerosis and Alzheimer’s disease.
One notable feature of the BBB is the elevated mitochondrial content compared with peripheral endothelial cells, which form the inner lining of blood vessels. While mitochondrial dysfunction has been associated with neurodevelopmental and neurodegenerative disorders, little is known about its role in the BBB. To explore this in greater detail, researchers decided to focus on 22qDS, also known as DiGeorge syndrome. This genetic condition, involving six mitochondrial genes, raises the risk for neurodevelopmental and neurodegenerative diseases. Patients have a 25-fold increased risk of developing psychosis, and one in four individuals with this syndrome develop schizophrenia.
CHOP has the world’s largest clinic dedicated to the care of children, adolescents and some adults with 22qDS, and a dedicated team of researchers at Penn and CHOP studies the condition as a window into the deeper mysteries of neurodevelopmental disease.
We previously established that the BBB is compromised in 22qDS, indicating that the crosstalk between the brain and the periphery can be affected. With these findings in mind, we addressed the hypothesis that mitochondrial deficits contribute to BBB dysfunction in 22qDS.”
Jorge Iván Alvarez, PhD, co-senior study author, associate professor of pathobiology at Penn Vet
“This study really demonstrates the power of collaboration,” said co-senior study author Stewart A. Anderson, MD, Associate Chair for Research in the department of Child and Adolescent Psychiatry and Behavioral Sciences at CHOP and associate director of the CHOP/Penn Lifespan Brain Institute. “By combining our respective expertise on mitochondrial function and the BBB, we have made an important discovery that may substantially help individuals with 22qDS.”
The researchers indeed found impairment, suggesting a “leaky” BBB, using a combination of human induced pluripotent stem cell-derived brain microvascular endothelial cells from patients with 22qDS and in BBB endothelial cells from a preclinical model of 22qDS.
Perhaps most exciting, the researchers found that treatment with the drug bezafibrate, a cholesterol drug that is also an activator of mitochondrial generation and turnover, can enhance BBB function in both the stem cell system and in the preclinical model of 22qDS. Treatment in the preclinical model also corrected their deficit in social memory, an abnormality associated with BBB dysfunction as well as schizophrenia. These findings suggest that this class of drugs could potentially be repurposed if the findings are confirmed in clinical trials. While 22qDS was the focus of this study, Drs. Anderson and Alvarez and their teams believe that the findings may have implications for the targetable role of mitochondrial dysfunction in the BBB in other neuropsychiatric conditions, including the development of psychosis outside of the context of 22qDS.
This study was supported by the Uytengsu-Hamilton 22q11 Neuropsychiatry Research Program of the Maternal and Child Health Research Institute (MCHRI) at Stanford University UH22QEXTFY22-03; the National Institutes of Health (NIH) grant to the Institute of Translational Medicine and Therapeutics (ITMAT) and by the Transdisciplinary Awards Program in Translational Medicine and Therapeutics (TAPITMAT) of the University of Pennsylvania NCATS 5UL1TR001878-04; NIH grants R01MH134797-01, R01MH134893-01, R01MH110185-03, R01MH066912 and R37NS048471; the NIH–National Institute of Mental Health BRAIN initiative grant F32MH125600; the Penrose Family; the Howard Hughes Medical Institute; the Blavatnik Family Foundation graduate fellowship; the Multiple Sclerosis Canada–endMS Postdoctoral Fellowship; and the Brain and Behavior Research Foundation.
Source:
Journal reference:
Crockett, A. M., et al. (2025) Bezafibrate improves mitochondrial function, blood-brain barrier integrity and social deficits in models of 22q11.2 deletion syndrome. Science Translational Medicine. doi.org/10.1126/scitranslmed.ads2116.

