In an evolving health landscape, emerging research continues to highlight concerns that could impact everyday wellbeing. Here’s the key update you should know about:
A new radioimmunotherapy approach has the potential to cure human epidermal growth factor receptor 2 (HER2)-positive breast cancer, according to new research published in the November issue of The Journal of Nuclear Medicine. The regimen, which pre-treats the tumor before delivering targeted alpha-radioimmunotherapy, resulted in durable major responses–including histologic cures–with minimal toxicities, paving the way for a safer and more effective treatment option for breast cancer patients.
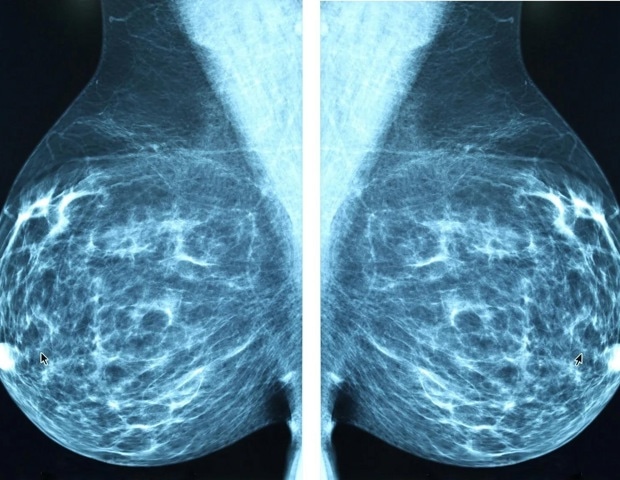
Advanced metastatic breast cancer has a poor prognosis, especially for highly aggressive HER2-positive subtypes. HER2 is an oncogene that is overexpressed in 15-20 percent of breast cancers and is a clinically established therapeutic target. Although current HER2-targeted therapies offer improved outcomes, challenges remain because of treatment-related adverse events and tumor resistance to treatment.
Previous studies have shown that HER2-targeted radioimmunotherapy with the α-particle-emitting radionuclide 225Ac has been effective, but not safe, as alpha-particles were retained in the body, resulting in high toxicities. In our study, we used a pretargeted radioimmunotherapy (PRIT) approach to directly treat the tumor and prevent potent alpha-particles from being absorbed in healthy tissues.”
Sarah Cheal, PhD, assistant professor at Weill Cornell Medicine, New York
The radioimmunotherapy treatment approach consisted of a three-step intravenous regimen: first a bispecific anti-HER2/anti-DOTA antibody, next a clearing agent, and finally 225Ac-Pr radioimmunotherapy. Researchers began by testing the effects of 225Ac-Pr dosing during PRIT on tumor-targeting efficiency and tissue biodistribution in a BT-474 breast cancer xenograft model. The regimen was then evaluated in mice bearing the BT-474 xenograft or a patient-derived xenograft. The mice were treated with either one or two cycles of 225Ac-PRIT separated by one week. A dose escalation study was also performed on the BT-474 model to establish the nephrotoxic absorbed radiation dose.
In the BT-474 model, 100 percent of mice achieved complete responses and 85 percent achieved histologic cure. One-cycle and two-cycle treatments were equally effective. Treatments were well tolerated, with no chronic radiation toxicity documented. In the patient-derived xenograft model, a single 225Ac-PRIT treatment led to 60 percent complete response and prolonged survival versus no treatment. Lastly, researchers identified the dose in the 225Ac-PRIT regimen at which severe chronic nephrotoxicity was induced.
“This study illustrates the curative potential of 225Ac-PRIT as a treatment for highly aggressive subtypes of HER2-positive breast cancer,” said Nai Kong Cheung, MD, PhD, member and attending physician in Pediatric Oncology at Memorial Sloan Kettering Cancer Center in New York. “If successfully translated to the clinic, HER2-directed 225Ac therapy could offer new treatment options in breast cancer and other HER2-expressing solid tumors.”
Source:
Journal reference:
Rinne, S. S., et al. (2025). 225Ac α-Pretargeted Radioimmunotherapy of Human Epidermal Growth Factor Receptor 2–Expressing Breast Cancer. Journal of Nuclear Medicine. doi: 10.2967/jnumed.125.269601. https://jnm.snmjournals.org/content/66/11/1714

