Stroke Damage Reversed As Stem Cells Regrow the Brain
Stem cell therapy reversed stroke damage in mice, regenerating neurons and restoring movement.
The findings bring scientists closer to human treatments that could one day transform recovery after brain injury.
Breakthrough in Stroke Recovery With Stem Cells
One in four adults suffer a stroke in their lifetime, leaving around half of them with residual damage such as paralysis or speech impairment because internal bleeding or a lack of oxygen supply kill brain cells irreversibly. No therapies currently exist to repair this kind of damage. “That’s why it is essential to pursue new therapeutic approaches to potential brain regeneration after diseases or accidents,” says Christian Tackenberg, the Scientific Head of Division in the Neurodegeneration Group at the University of Zurich (UZH) Institute for Regenerative Medicine.
Neural stem cells have the potential to regenerate brain tissue, as a team led by Tackenberg and postdoctoral researcher Rebecca Weber has now compellingly shown in two studies that were conducted in collaboration with a group headed by Ruslan Rust from the University of Southern California. “Our findings show that neural stem cells not only form new neurons, but also induce other regeneration processes,” Tackenberg says.
New Neurons From Human Stem Cells
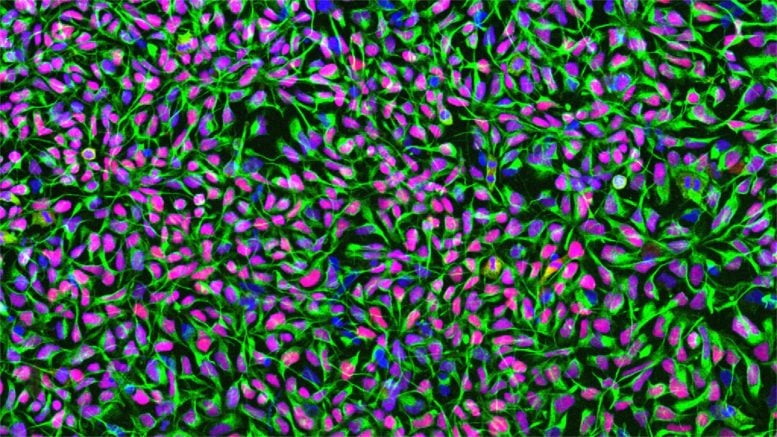
The studies employed human neural stem cells, from which different cell types of the nervous system can form. The stem cells were derived from induced pluripotent stem cells, which in turn can be manufactured from normal human somatic cells. For their investigation, the researchers induced a permanent stroke in mice, the characteristics of which closely resemble the manifestation of stroke in humans. The animals were genetically modified so that they would not reject the human stem cells.
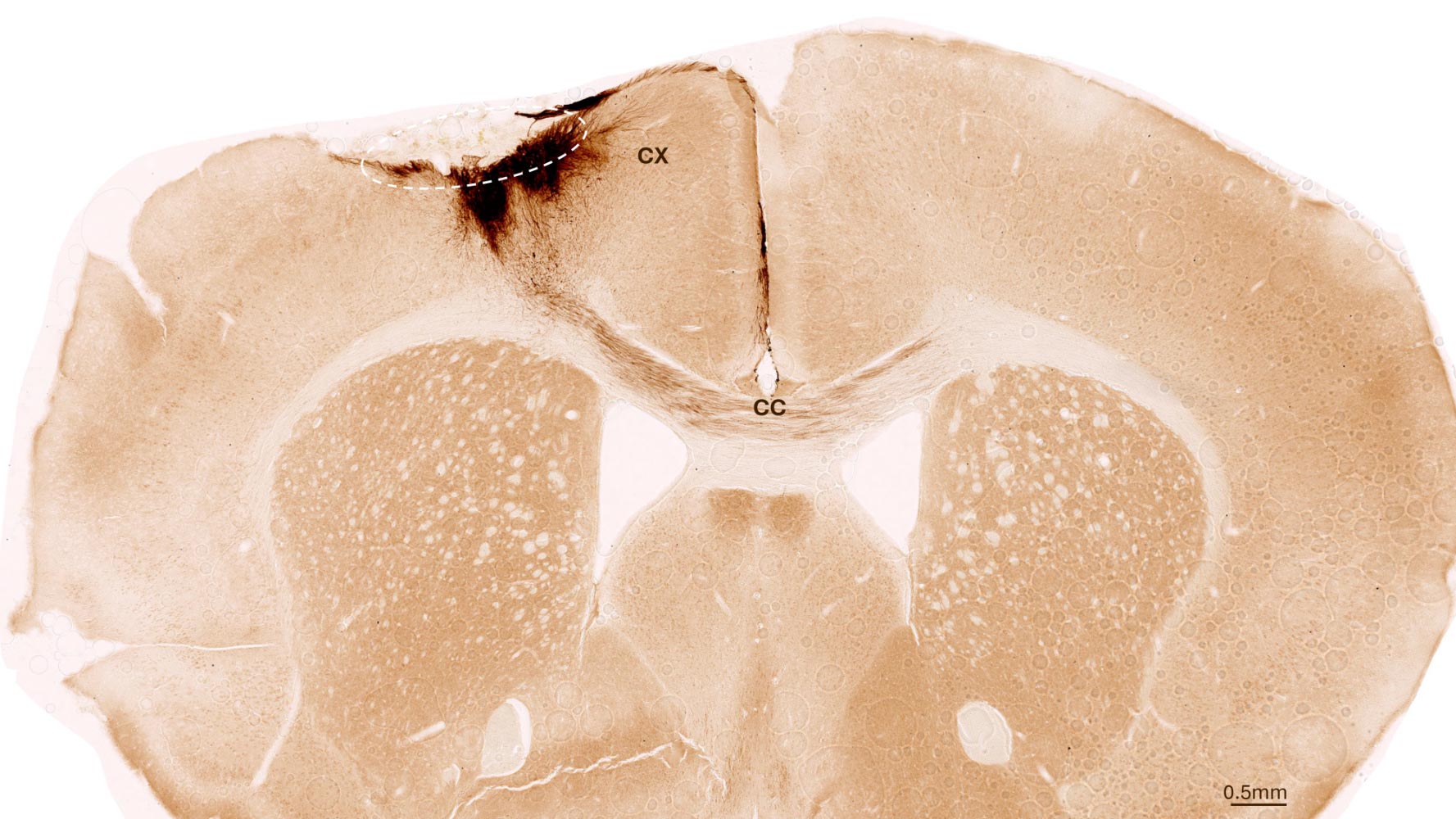
One week after stroke induction, the research team transplanted neural stem cells into the injured brain region and observed subsequent developments using a variety of imaging and biochemical methods. “We found that the stem cells survived for the full analysis period of five weeks and that most of them transformed into neurons, which actually even communicated with the already existing brain cells,” Tackenberg says.
Brain Regeneration Beyond Neurons
The researchers also found other markers of regeneration: new formation of blood vessels, an attenuation of inflammatory response processes, and improved blood-brain barrier integrity. “Our analysis goes far beyond the scope of other studies, which focused on the immediate effects right after transplantation,” Tackenberg explains. Fortunately, stem cell transplantation in mice also reversed motor impairments caused by stroke. Proof of that was delivered in part by an AI-assisted mouse gait analysis.
Clinical Application Moving Closer to Reality
When he was designing the studies, Tackenberg already had his sights set on clinical applications in humans. That’s why, for example, the stem cells were manufactured without the use of reagents derived from animals. The Zurich-based research team developed a defined protocol for that purpose in collaboration with the Center for iPS Cell Research and Application (CiRA) at Kyoto University. This is important for potential therapeutic applications in humans. Another new insight discovered was that stem cell transplantation works better when it is performed not immediately after a stroke but a week later, as the second study verified. In the clinical setting, that time window could greatly facilitate therapy preparation and implementation.
Challenges, Safety Measures, and Future Outlook
Despite the encouraging results of the studies, Tackenberg warns that there is still work to be done. “We need to minimize risks and simplify a potential application in humans,” he says. Tackenberg’s group, again in collaboration with Ruslan Rust, is currently working on a kind of safety switch system that prevents the uncontrolled growth of stem cells in the brain. Delivery of stem cells through endovascular injection, which would be much more practicable than a brain graft, is also under development. Initial clinical trials using induced stem cells to treat Parkinson’s disease in humans are already underway in Japan, Tackenberg reports. “Stroke could be one of the next diseases for which a clinical trial becomes possible.”
Reference: “Neural xenografts contribute to long-term recovery in stroke via molecular graft-host crosstalk” by Rebecca Z. Weber, Beatriz Achón Buil, Nora H. Rentsch, Patrick Perron, Stefanie Halliday, Allison Bosworth, Mingzi Zhang, Kassandra Kisler, Chantal Bodenmann, Kathrin J. Zürcher, Daniela Uhr, Debora Meier, Siri L. Peter, Melanie Generali, Shuo Lin, Markus A. Rüegg, Roger M. Nitsch, Christian Tackenberg and Ruslan Rust, 16 September 2025, Nature Communications.
DOI: 10.1038/s41467-025-63725-3
Never miss a breakthrough: Join the SciTechDaily newsletter.
Follow us on Google, Discover, and News.
Source link

