Tiny Lab-Grown Spinal Cords Could Hold the Key to Healing Paralysis

Researchers have created a remarkable new approach to repairing spinal cord injuries by merging 3D printing, stem cells, and lab-grown tissues.
They engineered tiny scaffolds that guide stem cells to form nerve fibers capable of bridging severed spinal cords. In experiments with rats, this method restored nerve connections and movement, offering new hope that one day similar techniques could help people living with paralysis.
Breakthrough in Spinal Cord Injury Treatment
For the first time, scientists at the University of Minnesota Twin Cities have successfully combined 3D printing, stem cell science, and lab-grown tissues to explore a new approach for treating spinal cord injuries.
Details of the work appear in the journal Advanced Healthcare Materials, a peer-reviewed scientific journal.
Spinal cord injuries affect more than 300,000 people in the United States, according to the National Spinal Cord Injury Statistical Center. There is still no treatment that can fully reverse the paralysis and long-term damage these injuries cause. One of the biggest barriers to recovery is that nerve cells die, and the remaining fibers cannot regrow across the site of injury. The Minnesota team designed their study to directly address this challenge.
3D-Printed Scaffolds and Stem Cells
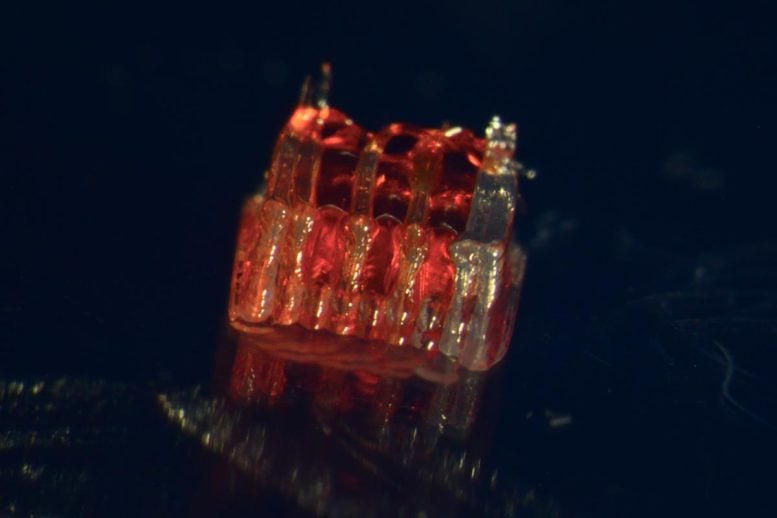
The researchers developed a specialized 3D-printed structure known as an organoid scaffold. This tiny framework contains microscopic channels that are filled with spinal neural progenitor cells (sNPCs). These cells, which originate from human adult stem cells, can divide and develop into specific types of mature nerve cells.
“We use the 3D printed channels of the scaffold to direct the growth of the stem cells, which ensures the new nerve fibers grow in the desired way,” said Guebum Han, a former University of Minnesota mechanical engineering postdoctoral researcher and first author on the paper who currently works at Intel Corporation. “This method creates a relay system that when placed in the spinal cord bypasses the damaged area.”
Successful Transplants in Animal Models
In their study, the researchers transplanted these scaffolds into rats with spinal cords that were completely severed. The cells successfully differentiated into neurons and extended their nerve fibers in both directions—rostral (toward the head) and caudal (toward the tail)—to form new connections with the host’s existing nerve circuits.
The new nerve cells integrated seamlessly into the host spinal cord tissue over time, leading to significant functional recovery in the rats.
The method involves creating a unique 3D-printed framework for lab-grown organs, called an organoid scaffold, with microscopic channels. Credit: McAlpine Research Group, University of Minnesota
Toward Future Clinical Translation
“Regenerative medicine has brought about a new era in spinal cord injury research,” said Ann Parr, professor of neurosurgery at the University of Minnesota. “Our laboratory is excited to explore the future potential of our ‘mini spinal cords’ for clinical translation.”
While the research is in its beginning stages, it offers a new avenue of hope for those with spinal cord injuries. The team hopes to scale up production and continue developing this combination of technologies for future clinical applications.
Reference: “3D-Printed Scaffolds Promote Enhanced Spinal Organoid Formation for Use in Spinal Cord Injury” by Guebum Han, Nicolas S. Lavoie, Nandadevi Patil, Olivia G. Korenfeld, Hyunjun Kim, Manuel Esguerra, Daeha Joung, Michael C. McAlpine and Ann M. Parr, 23 July 2025, Advanced Healthcare Materials.
DOI: 10.1002/adhm.202404817
In addition to Han and Parr, the team included Hyunjun Kim and Michael McAlpine from the University of Minnesota Department of Mechanical Engineering; Nicolas S. Lavoie, Nandadevi Patil and Olivia G. Korenfeld from the University of Minnesota Department of Neurosurgery; Manuel Esguerra from the University of Minnesota Department of Neuroscience; and Daeha Joung from the Department of Physics at Virginia Commonwealth University.
This work was funded by the National Institutes of Health, the State of Minnesota Spinal Cord Injury and Traumatic Brain Injury Research Grant Program and the Spinal Cord Society.
Never miss a breakthrough: Join the SciTechDaily newsletter.
Source link

