I (Katelyn) have escaped to the Amazon, where the internet cannot even reach me. So this week, I left the YLE keys with my team and our good friend—and scientific communication rockstar—Dr. Jess Steier. You’re in good hands. Jess, take it away…
I have two kids in elementary school, a petri dish if there ever was one. Every day during flu season feels like a game of Russian roulette. My husband (an ER doc), the kids, and I got our flu shots before Halloween—we follow the “flu before boo” guidance, though it’s not too late if you haven’t gotten yours yet. We’ve had a few colds this season, but have miraculously dodged the flu so far, even as it tears through their school like a rumor in the cafeteria.
With flu activity surging, so are the questions (including from YLE readers), falsehoods, and concerns about antivirals. One viral TikTok blames Tamiflu for a child’s hallucinations, but the flu itself is a much more likely cause. A popular homeopathic account shared a “Tamiflu tea” recipe (an herbal drink with no proven antiviral effect) to nearly half a million followers. Posts warning parents to “never take Tamiflu” are racking up thousands of likes.
It’s scary to see your child sick, and you want to make the right decisions in a world saturated with conflicting information. So let’s cut through the noise.
Before we begin, though, a quick note: This isn’t meant to be medical advice (we can’t diagnose you), and you should consult with a clinician for any diagnosis or treatment advice.
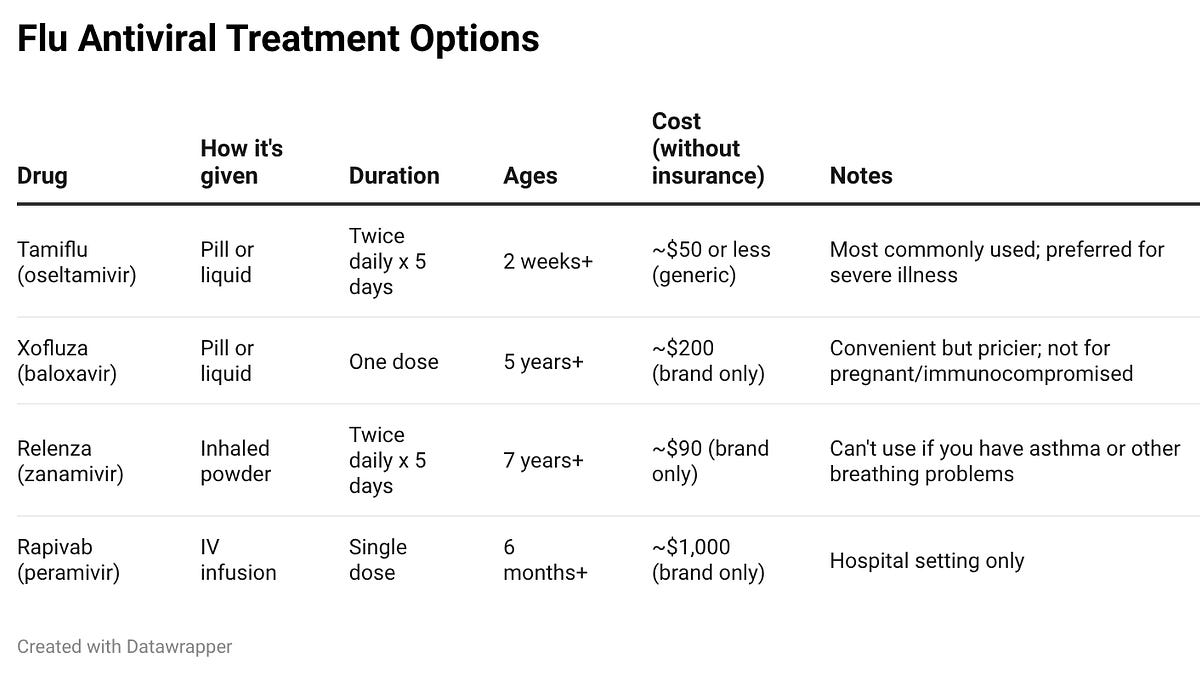
There are four FDA-approved antiviral medications for flu. All require a prescription. Here’s a quick rundown:
For most of us, we’ll be choosing between Tamiflu and Xofluza. The others have specific limitations—Relenza requires an inhaler device and isn’t safe for people with respiratory conditions, and Rapivab is IV-only, typically reserved for hospitalized patients.
Here’s what antivirals can do:
-
Shorten illness (how long you’re sick) by about one to two days (potentially three days in young kids when started within 12 hours of infection)
-
Reduce severity of symptoms (how crappy you feel) and risk of certain complications (e.g., ear infections in kids)
-
Reduce risk of death in high-risk groups (especially older adults)
-
Prevent flu after a known exposure (if someone in your household has the flu, taking antivirals right away can cut your risk of symptomatic flu in half)
Here’s what they can’t do: work magic if you wait too long. These medications work best when started within 48 hours of symptom onset, though people with severe illness or high-risk conditions may still benefit even if treatment starts later. If you are at increased risk of severe flu and you are exposed to it, you should not wait until you have severe symptoms before requesting antivirals—the earlier they are taken, the better off you will be, even if you don’t have symptoms yet. (This is a general rule for all antiviral medications.) Don’t sit on it hoping things improve.
Flu tends to hit hard and fast—sudden high fever, significant body aches, exhaustion that knocks you flat. Colds usually come on more gradually with milder symptoms. If you feel like you got hit by a truck out of nowhere, think flu. That said, flu and Covid can look a lot alike, and both have antivirals that work best when started early—but they’re different drugs. (Tamiflu won’t help Covid, and Paxlovid won’t help flu.) Many at-home tests now check for both, and test-to-treat programs (like this one, at CVS) can help sort out which virus you’re dealing with and get you the right treatment.
Like any medication, flu antivirals can cause side effects, but for most people, they’re mild and temporary. The most common issues are gastrointestinal, especially nausea and vomiting, particularly with Tamiflu. Taking it with food can help. Headaches can also happen. Serious side effects are rare, and most people complete the five‑day course without needing to stop the medication. For most high-risk people, the benefits of preventing flu complications outweigh these potential side effects.
Not everyone with the flu needs an antiviral. For many healthy older kids and adults, rest, fluids, and fever reducers will get you through just fine. Adding a medication that might cause nausea or vomiting isn’t always worth it.
But for some people, antivirals aren’t optional—they’re an important tool to prevent serious complications.
The American Academy of Pediatrics (AAP) and the Infectious Diseases Society of America (IDSA) recommend antiviral treatment for:
-
Anyone hospitalized with flu
-
Anyone with severe or worsening illness
-
Kids under 5 (especially under 2)
-
Adults 65+
-
Pregnant women
-
Anyone who is immunocompromised
-
People with underlying conditions like asthma, diabetes, or heart disease
If you or your child falls into one of these groups, don’t wait. Call your doctor or use a test-to-treat program at a pharmacy or clinic, where you can get tested, be seen by a clinician, and receive medication on the spot. If you’re not sure whether you or your loved ones fit into one of these groups, it’s worth speaking with a prescriber about whether or not to get treatment.
Tamiflu is the workhorse. It’s been around for decades, we have extensive safety data (including in babies as young as two weeks), and it’s available as a cheap generic.
But you have to take it twice daily for five days (if you have symptoms; if you are taking it as prevention, it is once daily), and about one in five people experience nausea or vomiting (GI upset). It’s the preferred choice for individuals who have severe illness, are at high-risk for complications, or are hospitalized.
Resistance to Tamiflu can occur, but tends to be rare—though we have had flu epidemics in the past with resistant viruses.
Xofluza is newer. One dose and you’re done. Less GI upset. Clinical trial data suggest it may stop viral shedding faster—around one day vs. three days with Tamiflu. This means people taking Xofluza may be contagious for a shorter period of time, be able to return to school or work sooner, and be less likely to spread the flu to household members than those taking Tamiflu. And Xofluza may work better than Tamiflu against influenza B.
But it’s pricier, and insurance coverage is limited. Less than half of Medicare plans and ACA marketplace plans cover it, and many Medicaid plans require prior authorization. Availability has been a real problem this season. (We’ve heard from many of you struggling to find it.) We also lack evidence to support its use among those pregnant or breastfeeding, in children under age 12, and those who are immunocompromised. This does NOT mean it doesn’t work in these populations or that it’s unsafe—it reflects the relative novelty of the drug.
Finally, there’s a chance the virus can become resistant to medication. (This seems more likely with H3N2 strains than with H1N1, and more likely in younger kids). If resistant strains start to circulate more widely, the medication might become less effective for others who get infected with the resistant strain. For these reasons, many clinicians still default to Tamiflu.
Want a quick visual summary? My team at Unbiased Science put together a post that walks through the key points about flu antivirals:
The falsehoods circulating right now hit on a few specific fears. Let’s address them directly.
“Tamiflu causes hallucinations and makes people suicidal.” There have been rare reports of neuropsychiatric effects—mostly from Japan, mostly in adolescents. The FDA added a warning to the drug label about this in 2006. But a subsequent 2008 Japanese review of over 10,000 children and adolescents found no evidence that Tamiflu caused abnormal behavior. An even more recent study of nearly 700,000 children showed that use of Tamiflu was actually associated with a lower risk of neuropsychiatric manifestations in children. This suggests that the more likely explanation for these events is that they were caused by flu directly, and Tamiflu was not effective enough at preventing them. Yes, the flu itself can cause delirium, confusion, and neurological symptoms. Though rare, it’s more common in kids with high fevers. Teasing apart drug effects from disease effects is genuinely difficult. After millions of doses worldwide, serious negative effects remain rare. The known risks of flu complications in high-risk groups—hospitalization, pneumonia, death—are not.
“Tamiflu is made from star anise, so just make star anise tea.” This one has a kernel of truth but misses the mark. Tamiflu was originally derived from shikimic acid, found in star anise. But shikimic acid is just a starting material; it undergoes extensive chemical processing in a lab to become oseltamivir, a completely different molecule. Consuming star anise to get Tamiflu is like eating flour hoping to get bread. If warm tea and honey bring you comfort when you’re sick, great. (Note: do NOT give honey to kids under 12 months of age.) But it’s not a substitute for antivirals when your clinician recommends them.
“Tamiflu is ineffective.” Tamiflu is extremely effective when used for the right patients at the right time, as long as the viruses are not resistant. The challenge is that flu moves so quickly that getting it early enough to make a difference can be tough. There’s solid evidence that it can prevent certain flu complications, such as ear infections, and shorten the duration of illness. It’s less clear how well it protects against hospitalization and death from flu, though observational studies are supportive. The earlier it’s started, the better it works—and this is particularly important for those at high risk for severe flu. However, it does have some side effects (the main one being nausea), which means it might not be worth it for low-risk people who will almost certainly recover on their own, especially if many days have passed since symptoms started.
If you or your child gets sick:
-
Get tested early. Many pharmacies and clinics offer test-to-treat programs.
-
If you’re high-risk, start antivirals within 48 hours; don’t wait to “see how it goes.”
-
If you’re not high-risk, talk to your clinician about whether treatment makes sense for your situation.
If you’re seeing scary claims online:
-
A scary story can feel compelling, but rare side effects get amplified online precisely because they’re unusual, not because they’re typical.
-
Consider the source. Is this someone with relevant expertise, or a wellness influencer?
-
Vetting sources can be tricky, but look for red flags: Are they selling a product or sharing a referral link? Do their claims contradict what major medical organizations recommend? Remember, the wellness industry is a multi-trillion-dollar market. A lot of anti-pharma content is really just pro-alternative-pharma content.
Flu antivirals are a useful tool—not a miracle cure, but not something to fear either. They work best when started early by people who need them most. The evidence supports their use in high-risk groups to reduce complications and severity. For everyone else, they’re an option worth discussing with your clinician. Don’t forget to ask about other members of your household who might be at high risk for severe flu and whether they should consider taking antivirals preventively.
Still, none of this is a substitute for vaccination. Getting the flu shot won’t always prevent infection, but it significantly reduces your risk of severe illness, hospitalization, and death. Add in good ventilation, masking, and handwashing. But when flu breaks through, antivirals are a valuable backup—and the best one is the one you can start quickly.
Stay safe out there.
Love,
Jess
Dr. Jess Steier, DrPH, is a public health scientist and founder of Unbiased Science. Your Local Epidemiologist (YLE) is founded and operated by Dr. Katelyn Jetelina, MPH PhD—an epidemiologist, wife, and mom of two little girls. YLE reaches more than 425,000 people in over 132 countries with one goal: “Translate” the ever-evolving public health science so that people will be well-equipped to make evidence-based decisions. This newsletter is free to everyone, thanks to the generous support of fellow YLE community members. To support the effort, subscribe or upgrade below:

