In an evolving health landscape, emerging research continues to highlight concerns that could impact everyday wellbeing. Here’s the key update you should know about:
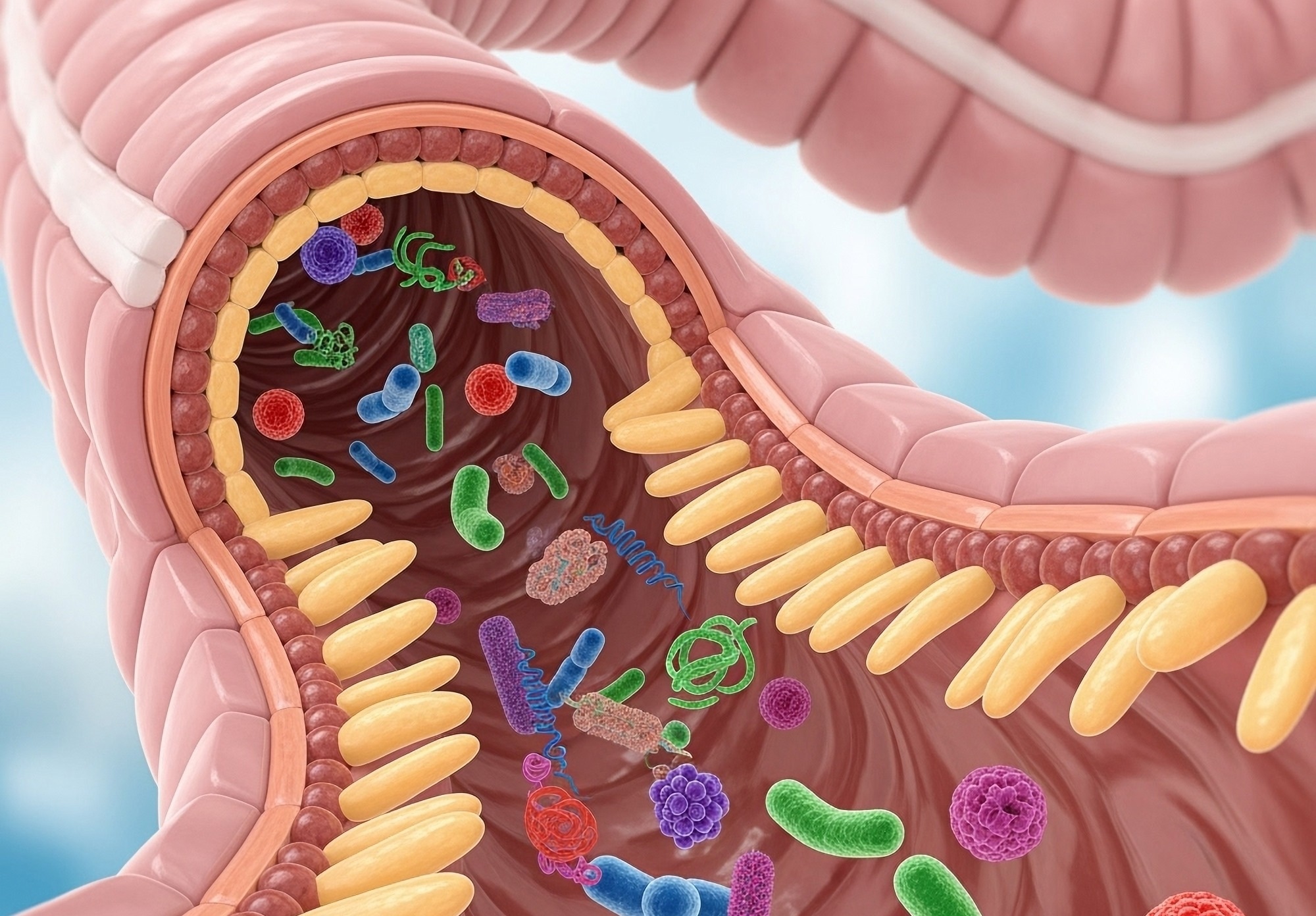
Study: From obesity to cancer: Gut microbiome mechanisms, biomarkers, and U.S. public health strategies. Image Credit: Shutterstock AI Generator / Shutterstock.com
A recent review published in Oncoscience reveals that the gut microbiome serves as both a biomarker and therapeutic target in diseases like obesity, metabolic syndrome, and colorectal cancer (CRC).
The role of the gut microbiome in common diseases
Metabolic syndrome, obesity, and CRC are among the most common health challenges in the United States. Current estimates suggest that 40% of U.S. adults are currently obese, which increases their risk of cardiovascular disease, type 2 diabetes, and cancer.
CRC is the second leading cause of cancer death in the U.S. and is strongly associated with dietary and lifestyle factors. Obesity and CRC are major sources of health care expenditure and mortality, thus emphasizing the urgent need for effective approaches to prevent and manage these diseases within diverse U.S. populations.
The gut microbiome consists of bacteria, archaea, fungi, and viruses that inhabit the digestive tracts of humans and animals. These intestinal microorganisms play a crucial role in host metabolism, immunity, and carcinogenesis, with gut dysbiosis often observed in obesity, chronic low-grade inflammation, and insulin resistance.
The Nurses’ Health and Health Professionals Follow-up studies revealed that specific microbial signatures correlate with CRC risk and obesity phenotypes. Similarly, the National Health and Nutrition Examination Survey (NHANES) has established the role of gut microbial composition in shaping metabolic health.
Mechanistic insights into how the gut microbiome impacts disease risk
Metagenomic analyses have revealed that the gut microbiome of obese individuals exhibits increased metabolic capacity for harvesting energy from otherwise indigestible polysaccharides. Nevertheless, due to the heterogeneity of human microbiomes across diverse dietary, ethnic, and geographic backgrounds, additional research is needed to establish universal and population-specific microbial patterns linked to obesity.
Microbial metabolites, particularly short-chain fatty acids (SCFAs) like butyrate, acetate, and propionate, are implicated in metabolic health. SCFAs improve gut barrier function, regulate appetite, and modulate insulin sensitivity through G-protein-coupled receptors, with alterations in SCFA profiles correlating with lipogenesis and impaired gut barrier integrity.
Microbial dysbiosis promotes endotoxemia by increasing the abundance of Gram-negative pathogenic bacteria and circulating lipopolysaccharides (LPS) levels. The accompanying induction of toll-like receptor 4 (TLR4) signalling also enhances insulin resistance in adipose and hepatic tissues.
Chronic activation of LPS, TLRs, flagellin, mitogen-activated protein kinase (MAPK), and nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) facilitates the secretion of proinflammatory cytokines, which sustain a pro-tumorigenic microenvironment. Moreover, SCFAs, particularly butyrate, act as histone deacetylase (HDAC) inhibitors, thereby modulating gene transcription.
Multiple studies have highlighted the dual role of microbial metabolites in both preventing and promoting mutagenesis. Whereas butyrate promotes apoptosis in cancer cells and supports epithelial barrier integrity in healthy tissue, colibactin, which is produced by certain Escherichia coli species, causes DNA strand breaks and fosters mutagenesis.
Recent U.S.-based studies have combined metagenomics, metabolomics, and transcriptomics data to establish the role of functional microbial pathways and taxonomic composition in various diseases. Multi-omics strategies have played a vital role in developing microbiome-informed diagnostics and personalized prevention strategies. Researchers have combined electronic health records with multi-omics data to predict disease risk, thereby transforming screening and prevention approaches.
In addition to microbial composition and host genetics, environmental factors like air pollution, as well as diet, smoking habits, sleep patterns, physical activities, and other lifestyle factors significantly influence the microbiome and associated disease mechanisms. A clear understanding of these modifiers enables researchers and clinicians to design more effective personalized prevention strategies linked with microbiome science and environmental health.
Molecular pathological epidemiology (MPE) is a powerful integrative framework that combines molecular pathology with epidemiologic and bioinformatic approaches to understand disease heterogeneity driven by interactions among lifestyle, environmental, and genetic factors. Previously, MPE has been incorporated into gastrointestinal and colorectal cancer studies to investigate how microbial signatures, immune markers, and mutational profiles influence biological outcomes and therapy response.
Diagnostic and therapeutic potential of gut microbes
Stool-based microbiome profiling is a powerful diagnostic tool to detect CRC based on the presence of Fusobacterium nucleatum, colibactin-producing Escherichia coli, and enterotoxigenic Bacteroides fragilis. In fact, the integration of microbial markers with fecal immunochemical testing (FIT) has significantly improved the diagnosis of early-stage CRC.
Clinical studies have shown that the use of specific probiotic strains, including Bifidobacterium and Lactobacillus, has led to improvements in insulin sensitivity and reduced inflammation in obesity and metabolic syndrome. Inulin and resistant starch are prebiotics that promote the growth of beneficial taxa, including those that secrete butyrate with anticarcinogenic properties.
Gut dysbiosis can be restored through fecal microbiota transplantation (FMT). More recently, the U.S. Food and Drug Administration (FDA) approved the microbiota-based therapeutic RBX2660 (Rebyota®) for the first time to prevent recurrent Clostridium difficile infection.
Researchers are currently assessing the safety and efficacy of probiotics engineered for oncology and metabolic disorders. Preclinical studies indicate the potential of bacteriophage therapy targeting CRC-associated taxa, like Fusobacterium nucleatum.
Challenges and future prospects
Additional research is needed to translate microbiota-based therapeutics into clinical and public health practice. The lack of standardized methodologies across microbiome research limits reproducibility and cross-study comparisons. To overcome these challenges, novel approaches like the National Microbiome Data Collaborative have emerged to harmonize data standards, which could accelerate the translation into clinical settings.
In the future, large-scale longitudinal cohort studies must integrate microbiome, dietary, and lifestyle data to clarify temporal relationships. Clinical algorithms incorporating microbiome features are also crucial for validating diverse U.S. populations. Advanced technologies like artificial intelligence (AI) and machine learning models can also be used to combine microbiome, host genome, and metabolomic data to effectively predict disease risk.
Journal reference:
- Moseeb, M. H., Aizaz, M. M., Aiza, K., et al. (2025) From obesity to cancer: Gut microbiome mechanisms, biomarkers, and U.S. public health strategies. Oncoscience 12; 175-188. DOI: 10.18632/oncoscience.634. https://www.oncoscience.us/article/634/text/.