In an evolving health landscape, emerging research continues to highlight concerns that could impact everyday wellbeing. Here’s the key update you should know about:
A shoebox-sized optical device reads glucose directly through the skin in seconds, offering a promising step toward truly noninvasive, point-of-care glucose monitoring.
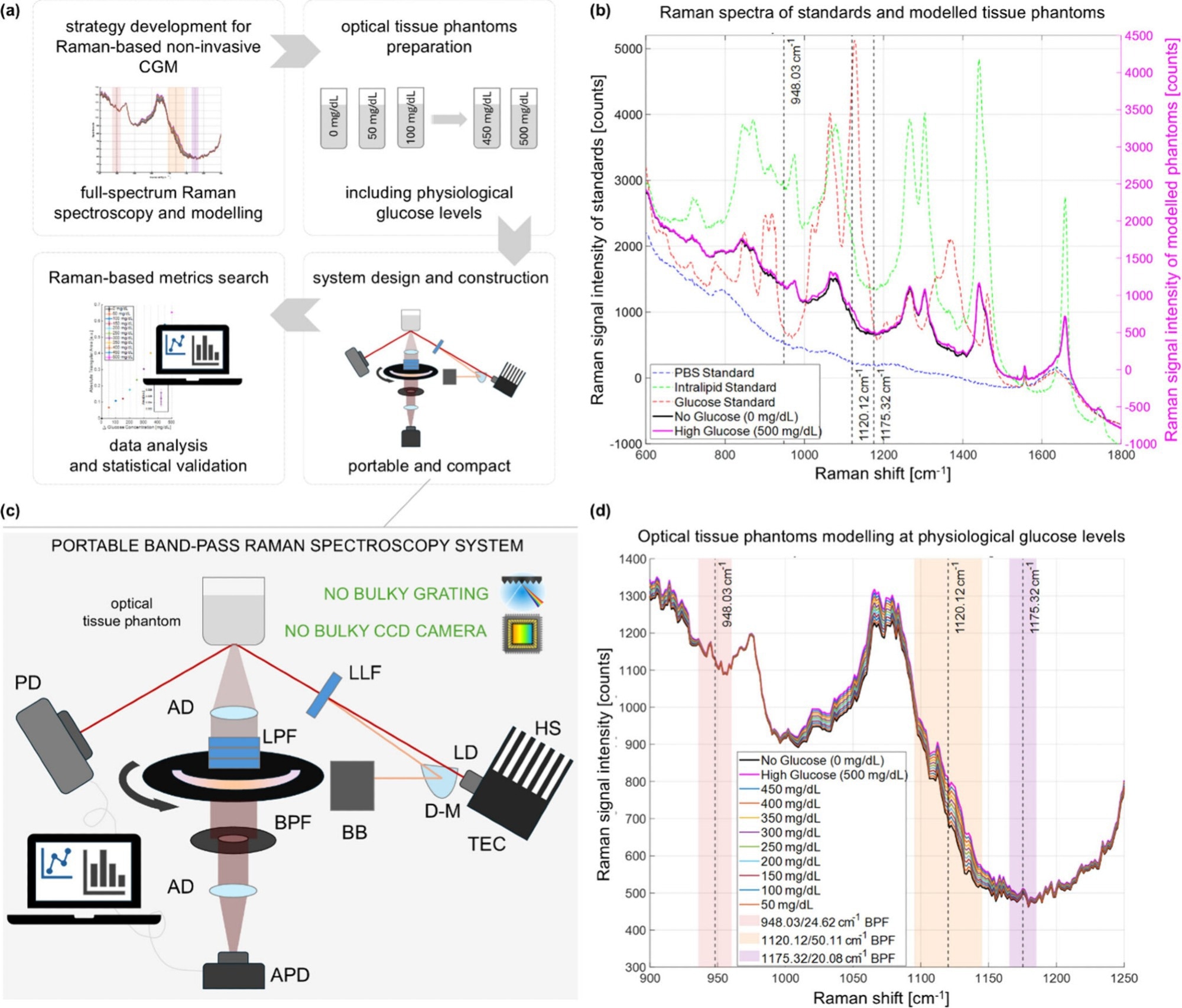
Pipeline for the development of compact BRS-based CGM. (a) Strategy development pipeline. (b) Measured full-spectrum Raman signal of individual components and modeled tissue phantom signals: PBS (blue line), 20% intralipid solution in water (green line); 20% glucose solution in water (red line); simulated no-glucose tissue phantom (black line); simulated high-glucose tissue phantom (pink line). (c) Scheme of the optical system for BRS. HS: heat sink; TEC: temperature control; D-M: D-shaped mirror; BB: beam blocker; LLF: laser line filter; AD: achromatic doublet; LPF: long-pass filter; BPF: band-pass filter; APD: amplified photodiode; PD: photodiode (d) Simulated Raman spectra around the Raman peak of glucose at 1125 cm–1 through 11 glucose levels. Shear areas indicate the chosen bands for BRS.
A recent study published in the journal Analytical Chemistry reports that Massachusetts Institute of Technology (MIT) researchers developed a noninvasive, light-based device that can accurately measure blood glucose levels in under a minute.
Global Need for Better Glucose Monitoring
Diabetes, a chronic metabolic condition characterized by elevated blood glucose levels, has become a significant public health crisis globally, with projections indicating 592 million cases by 2035. Effective and accurate monitoring of blood glucose is the cornerstone of diabetes treatment and management.
The traditional finger-pricking method has long been the standard approach, using lancets and test strips to measure capillary blood glucose. However, using this method every day, multiple times a day, is impractical for continuous glucose monitoring, leading to under-testing and an increased risk of severe health complications in people with diabetes.
Several wearable devices have also been developed for continuous glucose monitoring through sensors implanted just under the skin. These commercially available continuous glucose monitors rely on minimally invasive microneedles to measure glucose levels in interstitial fluid and typically need to be replaced every 10 to 14 days. However, these systems are not fully noninvasive and contribute to ongoing cost and device burden.
To overcome these limitations, several noninvasive methods have been developed, including vibrational spectroscopy that directly targets the molecular signatures of glucose, and photothermal and photoacoustic spectroscopy that analyze thermal or acoustic changes in tissue properties induced by glucose absorption.
Some indirect methods, such as photoplethysmography and breath analysis, have also emerged to monitor glucose levels by measuring secondary physiological effects or byproducts of glucose metabolism.
Many of these methods use artificial intelligence (AI) to process complex and noisy signals, which requires extensive training and may lack robustness and generalisability across different individuals and physiological conditions.
Introducing a Raman-Based Noninvasive Device
To address these challenges, MIT researchers developed a compact, noninvasive, portable sensor based on Raman spectroscopy using a band-pass Raman spectroscopy (BRS) approach for continuous glucose monitoring. Raman spectroscopy is a technique that shines near-infrared or visible light on tissues or cells to reveal their chemical compositions. The basic principle is to analyze how near-infrared or visible light is scattered, or deflected, as it encounters different kinds of molecules in tissues or cells.
Advancing Band-Pass Raman Spectroscopy
The researchers developed this Raman-based system to efficiently and accurately quantify glucose levels through optimized optics and physically interpretable spectral metrics. The system was mounted on breadboards and enclosed, resulting in a compact, portable glucose-monitoring device capable of directly measuring glucose Raman signals from the skin.
The glucose Raman signals, which were generated through near-infrared (830 nm) light, are generally too small to be easily distinguished from all other signals generated by cellular or tissue molecules. To filter out these unwanted signals, researchers shone near-infrared light onto the skin at an angle different from that used to collect the resulting Raman signal. This off-axis configuration suppresses elastically scattered light and enhances glucose-specific Raman features.
A Raman spectrum typically contains approximately 1,000 bands, which are spectral regions that correspond to specific molecular features. Among these bands, the researchers selected and analyzed only three strategically chosen spectral bands around the main glucose Raman peak, using two adjacent sidebands as intraspectrum references to measure blood glucose levels. This approach allowed them to measure with a cost-effective device about the size of a shoebox, without requiring full-spectrum acquisition or complex AI-driven models.
Testing and Validating the Prototype Device
The researchers conducted initial validation experiments using optical tissue phantoms across a wide range of glucose concentrations, followed by a pilot intraskin study to investigate the efficiency of this Raman-based portable system in continuously monitoring blood glucose levels in a human participant.
The study was conducted on a healthy male volunteer aged 27 years, who put his arm on the top of the device, and a near-infrared beam from the device shone through a small glass window onto the skin to perform the measurement. The measurements were taken every five minutes over a period of four hours.
For a comparative analysis, two commercially available, invasive continuous glucose monitors were inserted into the participant’s other arm to measure glucose levels every 5 minutes. A one-finger-prick standard glucometer was also used to measure blood glucose levels every 10 minutes.
To induce dynamic changes in blood glucose concentrations, the participant was instructed to drink two 75-gram glucose drinks during the trial. The final trial findings indicated that measurements from the Raman-based device closely tracked glucose trends and agreed with those from commercial invasive devices, with performance metrics comparable to those of current commercial continuous glucose monitors.
Implications for Future Glucose Monitoring
The portable, noninvasive Raman-based device developed in the study demonstrates promising preliminary performance for continuous monitoring of blood glucose levels, with measurement accuracy comparable to that of commercially available invasive glucose monitors in this pilot setting. The device takes approximately 36 seconds to complete a measurement, resulting in a total measurement time of under one minute.
While the current findings are based on a single healthy participant, these preliminary observations provide a strong basis for future studies with larger, more diverse populations, including people with diabetes, to better understand the potential of this point-of-care technology.
The device shows promise in transforming glucose monitoring, offering portability, accessibility, accuracy, and continuity for future clinical and personal health management applications, with the potential to reduce reliance on finger-prick testing and under-the-skin sensors over time.