I grew up in a family where most people worked in healthcare. I saw how they practiced, how manual and fragmented the work was, and how little support existed for mental health. Watching how far the field has come, and how far it still needs to go, has been fascinating to me.
Today, access has expanded, virtual appointments are now routine, evidence-based care is expected, and employers see mental health not as a side benefit but as a core driver of productivity, retention, and overall well-being. Technology has reshaped the way people engage with care, and cultural stigma has steadily given way to openness and demand.
But for all this progress, one thing hasn’t changed nearly enough: the structure of care itself. Mental health support is still delivered overwhelmingly as a series of discrete, episodic encounters. A person reaches out when something breaks, receives care for a period of time, and then slips back into the background of a fragmented system until the next crisis brings them back. It’s reactive by design, and costly, both emotionally and economically.
As the industry moves into its next chapter, the question is no longer simply how to expand access or digitize existing workflows. Those shifts have already reshaped the landscape. The real opportunity is to rebuild the care experience itself.
At Spring Health, we believe that the future is Continuous Care: a model where support surrounds the member, not the other way around. One where care is proactive rather than reactive, connected rather than episodic, and deeply personalized rather than one-size-fits-all. This model aims to deepen the therapeutic alliance with providers, ensuring members remain engaged and achieve significant progress before, during and in between their sessions.
This belief guided our work throughout 2025. And this year, we took our biggest steps yet toward making Continuous Care a reality.
Where We Started: Building Toward a New Model of Care
When we began investing in AI years ago, the goal wasn’t to build technology for its own sake. It was to solve real human problems in the care journey.
Healing doesn’t follow a weekly cadence. Between sessions, members often:
- Forget what they intended to discuss,
- Lose momentum after a breakthrough, or
- Disengage when life becomes overwhelming
Providers see these patterns every day, but without scalable tools, it’s nearly impossible to support every member between visits without increasing administrative or emotional burden.
So we asked a simple but transformative question:
What if care didn’t stop when the session ended?
We never saw AI as a replacement for empathy or therapeutic skill. We saw it as a way to help members stay oriented to their goals, feel grounded before sessions, and hold onto insights after. Our early work focused on empathy, risk identification, and navigation to build the clinician-supervised, safety-first foundation needed for something bigger.
That foundation set the stage for Continuous Care, a model that uses technology to integrate support before, during, and after every session.
What Continuous Care Is (and What It Isn’t)
Continuous Care doesn’t mean having a therapist on call 24/7.
It’s not asynchronous therapy, and it’s certainly not a replacement for the therapeutic relationship.
Instead, Continuous Care is about giving members the right kind of support between sessions to help them stay connected to their goals, build on the work they’re doing with their provider, and make steady, meaningful progress. It reinforces the therapeutic process rather than taking away from it.
At its core, Continuous Care reduces the friction and uncertainty that so many people feel throughout their journey. It helps avoid that familiar sense of “starting over” each week, and it creates a more seamless, grounded experience of care.
I like to think of Continuous Care as a way to better integrate the work more deliberately into everyday life to help people get better even faster.
What We Built in 2025 and What It Taught Us
This year, we expanded our member experience with features that start to bring our vision of Continuous Care to life: Guided Intake and Summaries & Takeaways. Together, these tools help members start therapy feeling more prepared and leave sessions with meaningful next steps, making progress easier to sustain.
Guided Intake: Starting Sessions Strong
In most mental healthcare delivery today, the first session is rarely where healing begins. It’s information gathering. Members spend much of that time retelling their story, answering the same questions they’ve discussed countless times before, and trying to remember what they wanted to say. Providers often describe first sessions as “administrative,” because they’re gathering history, clarifying goals, and piecing together context instead of getting into the work.
This isn’t a small problem. Research shows that individuals often feel anxious before a first appointment, and many leave feeling like they barely scratched the surface. Some become so overwhelmed at the thought of starting therapy that they don’t show up at all. For providers, these early sessions are essential but can also be inefficient. They’re necessary to establish understanding, yet they can delay momentum.
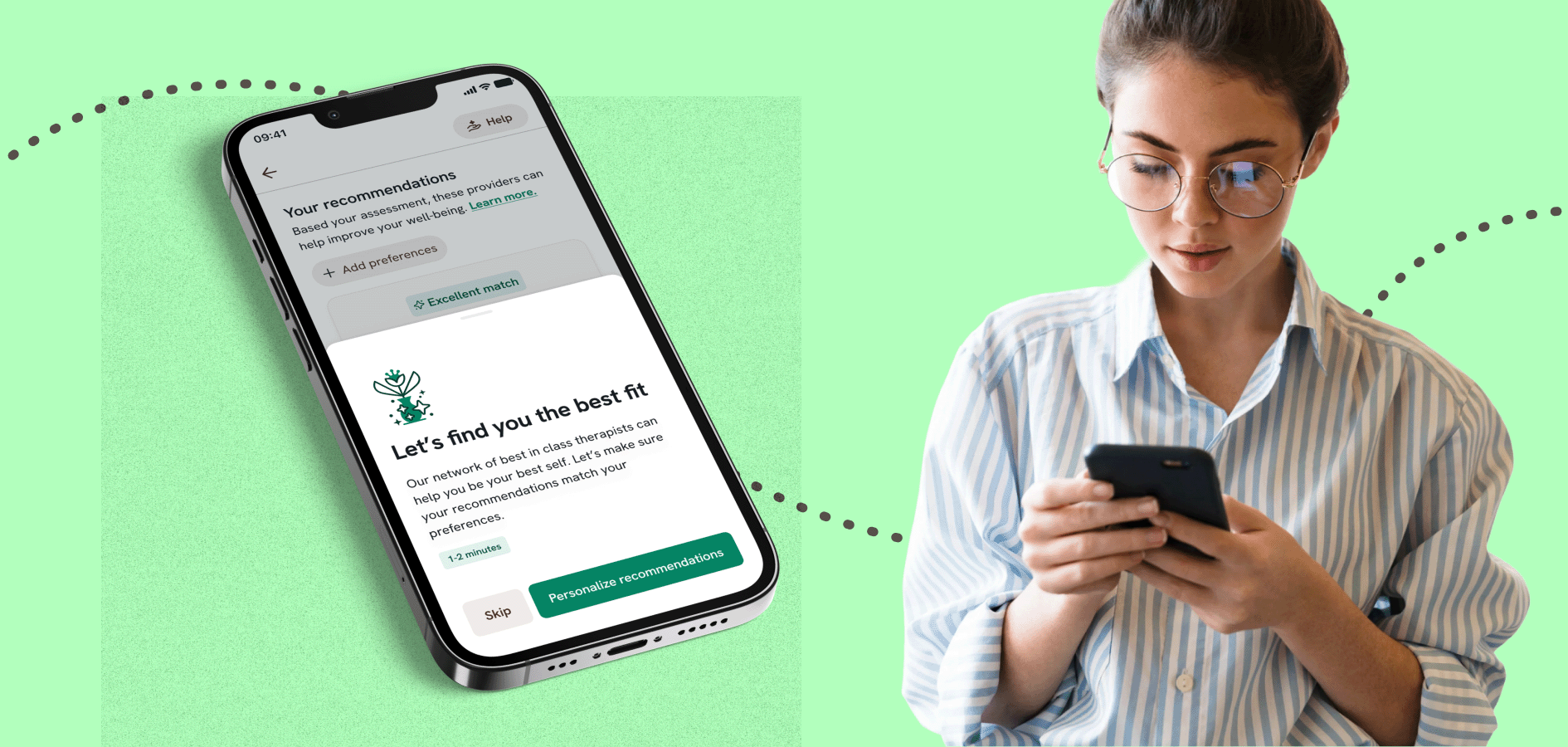
Guided Intake fundamentally changes the value of a first therapy appointment. Instead of walking into the first session cold, members have the time and space to reflect on what’s going on, what brought them to care, and what they hope to work on. Through a simple, conversational AI experience, they share their history and focus areas in a way that feels natural rather than clinical. They get a personalized summary of what they shared, and their provider receives that same information securely.
After engaging in the experience, one member shared, “This is the first time I had to pre-fill what my situation was before seeing a therapist. I feel like this will save time for the first session because they already have a heads up on my situation.”
Providers, in turn, enter the first session with a clearer, more complete picture of the member’s experience, allowing them to build rapport more quickly and begin the session with sharper focus.
This is a small but powerful example of Continuous Care in action: technology removing friction, strengthening the therapeutic bond, and enabling providers to spend their time on what matters most.
Summaries and Takeaways: Turning Sessions Into Lasting Progress
In traditional care, a session ends and patients are left on their own to process everything they just explored: what clicked, what mattered, what they want to try next. By the time the next session comes around, much of that clarity fades. Life gets busy. Insights get lost. And providers often hear the familiar phrase: “I know we talked about something important last week, but I can’t quite remember…”
This gap between sessions is one of the biggest drivers of stalled progress across the industry. Without structure or reminders, even highly motivated members struggle to translate in-session breakthroughs into real-life change.
With Summaries and Takeaways, members receive a personalized recap of the themes they explored after each session, along with simple, actionable next steps aligned with their therapeutic goals. They can revisit what they discussed, reflect on how things are going, and stay grounded in the work they’re doing.
Takeaways turn therapeutic guidance into bite-size actions: a grounding exercise to try before a stressful meeting, a small boundary-setting practice for the week, or a prompt to notice patterns or shifts in mood or behavior.
The impact is clear:
- Members stay more engaged between sessions,
- Their insight deepens as they revisit and reflect, and
- Progress accelerates because momentum isn’t lost
Providers see members showing up more prepared, more reflective, and more connected to their goals. Together, these capabilities transform the time between sessions from unstructured downtime into an active, supported part of the healing journey.
Responsible Innovation: The Spring Standard
As we build toward a new model of mental healthcare, the responsibility that comes with it only grows. Continuous Care can’t work without technology, but it also can’t rely on technology that isn’t safe, clinically aligned, or transparent. The industry is moving fast, and not always thoughtfully, which makes the bar for responsible innovation higher than ever.
As I’ve described before, our approach to AI is guided by five core principles to ensure it’s safe, ethical, and truly beneficial. These same principles can also help employers and health plans evaluate AI-powered solutions.
1. AI as an accelerator
AI enhances—never replaces—human care. It helps members access the right support faster and empowers providers to deliver higher quality care with less friction.
2. Privacy and security are foundational
Protecting member data is non-negotiable. Our AI operates within a secure, compliant infrastructure that meets the highest industry standards, including SOC 2, HITRUST, HIPAA, and GDPR, to maintain trust at every step.
3. Transparency and consent are built into care
Trust is essential. Members and providers always have clear visibility into when and how AI is used, and they can opt out at any time.
4. Safety and equity by design
AI must work for everyone. We rigorously test our models to ensure fairness, accuracy, and inclusivity across diverse populations, with oversight from our Internal AI Governance Board.
5. Continuous learning and improvement
AI isn’t static. As mental health needs evolve, so does our technology—continuously improving to drive better outcomes while upholding transparency and ethical responsibility.
As we apply these principles to Continuous Care, especially as AI begins supporting members between sessions, we also recognize the need for a clear, shared way to assess whether these technologies meet the clinical standards mental healthcare demands. Unlike other industries, mental health requires tools that can recognize nuance, uphold safety, and strengthen the therapeutic relationship rather than complicate it.
That’s why we developed VERA-MH (Validation of Ethical and Responsible AI in Mental Health): the first open-source, clinically grounded evaluation framework built for mental healthcare. VERA-MH establishes rigorous criteria for safety, crisis awareness, transparency, and ethical use. Created in partnership with clinicians, ethicists, suicide-prevention experts, and technologists, it offers a transparent benchmark that helps ensure AI supports members safely and effectively, without replacing the provider relationship or introducing unintended risks.
Why We Believe the Industry Needs Continuous Care
The reality is that many people still wait too long to get the right care, struggle to stay connected between sessions, and often feel alone in the moments when support could make the biggest difference. Continuous Care is designed to change that.
What we’re seeing so far is deeply encouraging: members are arriving more prepared, staying more engaged between sessions, and feeling more supported throughout their journey. Technology is helping them get more out of every session and strengthening the work they do with their provider.
And this is only the beginning. Continuous Care is how we’ll remove even more barriers and build a mental healthcare experience that truly meets people where they are and helps them move where they want to go.
Source link