In an evolving health landscape, emerging research continues to highlight concerns that could impact everyday wellbeing. Here’s the key update you should know about:
Scientists at Montefiore Einstein Comprehensive Cancer Center (MECCC) and Albert Einstein College of Medicine have shown for the first time that glioblastoma-the deadliest form of brain cancer-affects not just the brain but also erodes the skull, alters the makeup of skull marrow, and interferes with the body’s immune response. Drugs intended to inhibit skull-bone loss made the cancer more aggressive, according to results published today in Nature Neuroscience.
“Our discovery that this notoriously hard-to-treat brain cancer interacts with the body’s immune system may help explain why current therapies-all of them dealing with glioblastoma as a local disease-have failed, and it will hopefully lead to better treatment strategies,” said the paper’s corresponding author Jinan Behnan, Ph.D., assistant professor in the Leo M. Davidoff Department of Neurological Surgery and in the department of microbiology & immunology at Einstein, and a member of the National Cancer Institute (NCI)-designated MECCC.
According to the NCI, approximately 15,000 people are diagnosed with glioblastoma each year. The median survival of those who receive standard treatment of surgery, chemotherapy, and radiation is approximately 15 months.
A matter of marrow
As is true for many other bones, the skull contains marrow in which immune cells and other blood cells form. Dr. Behnan’s research on glioblastoma and the skull was prompted by recent studies revealing extremely thin channels that connect the skull with its underlying brain, allowing molecules and cells to travel between the skull’s marrow and the brain.
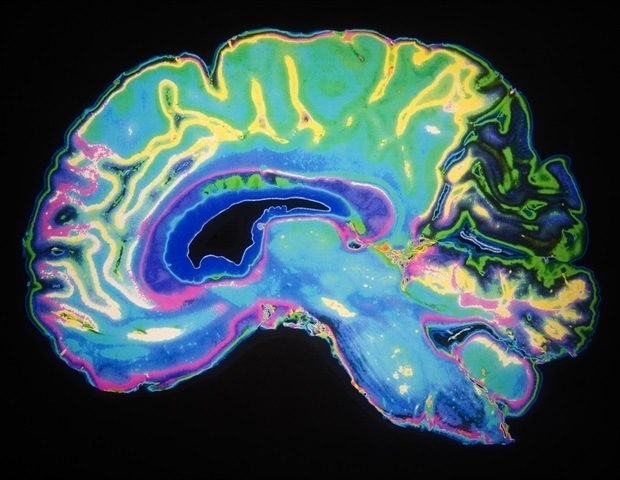
Dr. Behnan and colleagues used advanced imaging techniques on mice that developed two different types of glioblastomas. They found that the tumors caused skull bones to erode, especially along the sutures where skull bones fuse. Such erosions seem to be unique to glioblastoma and other malignant intracranial tumors, since they don’t occur with strokes, other types of brain damage, or even other systemic cancers. Computerized-tomography (CT) images of patients with glioblastoma revealed that decreases in skull thickness were present in the same anatomic areas as in mice.
The skull erosions in the mice were found to have increased the number and diameter of the skull-to-bone channels. The researchers hypothesized that these channels might allow the glioblastoma to transmit signals to the skull marrow that could profoundly change its immune landscape.
A tilt towards inflammation
Using single-cell RNA sequencing, the researchers found that glioblastoma had dramatically shifted the skull marrow’s immune-cell balance in favor of pro-inflammatory myeloid cells-nearly doubling the levels of inflammatory neutrophils, while nearly eliminating several types of antibody-producing B cells as well as other B cells.
“The skull-to-brain channels allow an influx of these numerous pro-inflammatory cells from the skull marrow to the tumor, rendering the glioblastoma increasingly aggressive and, all too often, untreatable,” said study co-author E. Richard Stanley, Ph.D., professor of developmental and molecular biology at Einstein.
This indicates the need for treatments that restore the normal balance of immune cells in the skull marrow of people with glioblastoma. One strategy would be suppressing the production of pro-inflammatory neutrophils and monocytes while at the same time restoring the production of T and B cells.”
E. Richard Stanley, Ph.D., Professor, Developmental and Molecular Biology, Montefiore Einstein Comprehensive Cancer Center
Interestingly, and adding to evidence that glioblastoma is a systemic rather than local disease, the marrows of the skull and femur reacted differently to the cancer. Glioblastoma activated several genes in the skull marrow that boosted production of inflammatory immune cells; but in femur marrow, the cancer suppressed genes needed to produce several types of immune cells.
The researchers wondered if administering anti-osteoporosis drugs that prevent bone loss would affect skull-bone erosion, glioblastoma, or both. To find out, they gave mice with glioblastoma tumors two different drugs approved by the U.S. Food and Drug Administration for treating osteoporosis. Both drugs (zoledronic acid and denosumab) halted skull erosion-but one of them (zoledronic acid) also fueled tumor progression in one type of glioblastoma. Both drugs also blocked the beneficial effects of anti-PD-L1, an immunotherapy drug that boosts levels of tumor-fighting T cells.
Source:
Journal reference:
Dubey, A., et al. (2025). Brain tumors induce widespread disruption of calvarial bone and alteration of skull marrow immune landscape. Nature Neuroscience. doi.org/10.1038/s41593-025-02064-4.